PDF version
What is Brugada syndrome?
Brugada syndrome is a rhythm disorder of the heart that can cause the bottom chambers of the heart (known as theventricles) to beat abnormally fast. When this occurs the heart becomes inefficient at pumping blood around the body. This can cause a person to feel dizzy, to faint or collapse and it can sometimes result in sudden death. Treatment is available once Brugada syndrome is diagnosed. However, a definite diagnosis can be difficult because not all people affected with Brugada syndrome display symptoms or classic ECG findings (see below).
Brugada syndrome is usually caused by an abnormality in the sodium channel. Every cell in the heart has channels, which allow molecules such as sodium, calcium and potassium to move in and out of the cells. The flow of these molecules controls the heart beat. In Brugada syndrome the sodium channel does not function correctly and sodium entering the cell is restricted.
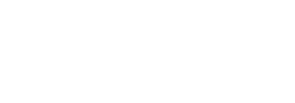
Usually, Brugada syndrome can be diagnosed on an electrocardiogram (ECG). There are three types of Brugada ECG patterns (Figure 1). The diagnosis of Brugada syndrome is only made if a person has a Type 1 Brugada pattern on their ECG either spontaneously or following infusion of flecainide. The Type 1 pattern should be demonstrated in at least one right praecordial lead (V1 or V2) placed in a standard or superior position (2nd, 3rd or 4th intercostal space). If a person is asymptomatic (i.e. has no symptoms) and only has a Type 2 or 3 change on their ECG, even following infusion of provocative drug (Eg flecainide), then they do not fulfil the criteria for the diagnosis of Brugada syndrome but they still require regular review by a cardiologist.
What causes Brugada syndrome?
Brugada syndrome is a genetic condition caused by a fault in a gene. Our body is made up of millions of cells. There are many different types of cells, including brain cells, liver cells and heart cells to name a few. Each cell contains 46 chromosomes, which hold the genetic material that decides features such as the colour of our eyes and whether we are tall or short. These 46 chromosomes are grouped into 23 pairs, one of each pair coming from mum and the other from dad. One of these pairs is known as the sex chromosomes – which decide whether we are male or female.
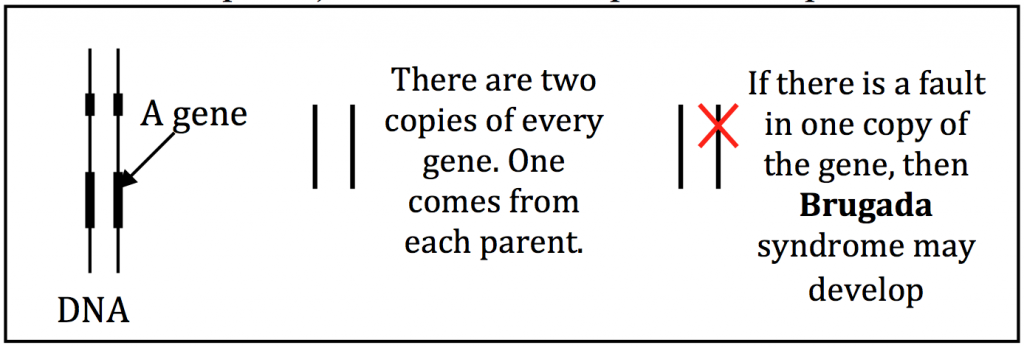
If you imagine a chromosome as being like a ball of wool, you could stretch it out into one long strand, which is known as the DNA. Along the length of DNA there are regions called genes. As there are two copies of every chromosome, there are also two copies of every gene (as mentioned, one from each parent). Genes act as recipes to make proteins in the body, and each recipe is unique based on the order of units. If there is a mistake in one of these genes (a mix-up in the order of these units) it may lead to the development of disease. This mistake is known as a gene fault.
In the case of Brugada syndrome we know of faults in at least 12 genes that can cause the condition. If there is a fault in one of these genes Brugada syndrome may result. Over 90% of identified gene faults known are in one particular gene called SCN5A that encodes the sodium channel.
How is Brugada syndrome inherited?
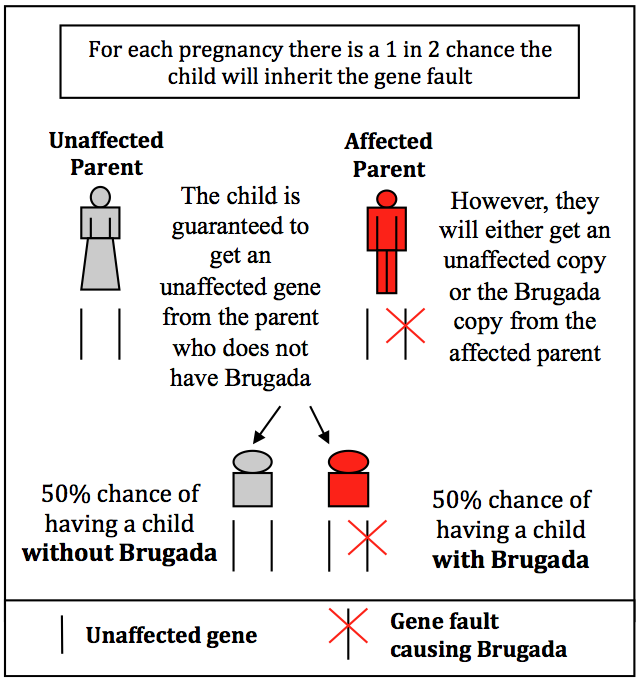
Brugada syndrome is known as an autosomal dominant condition, whereby the gene with the fault “dominates” over the unaffected gene to cause the condition. This means that an affected person has inherited one copy of the Brugada gene fault from one parent and one unaffected copy from the other parent. Likewise, if a person who carries the Brugada syndrome gene fault has a child, then the chance that the child will be affected is 50% or 1 in 2. This is because they are guaranteed to get an unaffected copy of the gene from the unaffected parent, but they can inherit either a Brugada copy or an unaffected copy from the parent with the condition. This is illustrated in the diagram.
On rare occasions, a person may have a gene alteration that has not been inherited from their parents. Instead, the alteration has arisen some time after conception. This means that their brothers and sisters are not likely to develop Brugada syndrome, however, the gene alteration can still be passed down to any children of the affected person.
What is genetic testing?
Genetic testing involves looking for the fault in the genes known to cause Brugada syndrome. It is a task that has been likened to looking for a single spelling mistake in a large book. Most families have their own unique gene fault. This may exist in one of the genes we have already identified or even in a gene that researchers have not yet linked to this condition. In an individual with Brugada syndrome, when they look for the gene fault in the most common gene (SCN5A), they find the gene fault that causes the condition in about 20-30% of families.
If genetic testing does not reveal a gene fault then we call this an inconclusive test result. This means that a gene fault most likely exists, but either our current technology is not yet good enough to detect the fault, or the fault is in a gene which has not yet been linked to Brugada syndrome.
If the gene fault is identified in the affected person then we can offer a gene test to other family members. This test takes 4-6 weeks for a result and will determine if the individual has inherited the Brugada gene fault or the unaffected copy of the gene. This is called predictive genetic testing, because it allows a person to know if they are likely to develop the condition even before symptoms are present. If they do not carry the gene fault then they will not develop Brugada syndrome, and future ECGs are not required. If they are shown to have the Brugada syndrome gene fault then there is a chance they will develop the condition and close follow-up by a cardiologist is recommended.
Genetic testing of the known Brugada syndrome genes is a commercial test. This means there is a cost involved and testing needs to be organised on a patient’s behalf by a doctor. If you would like to know more about centres offering commercial genetic testing, check the Cardiac Genetic Services around Australia, contact the Registry Coordinator on registry@centenary.org.au or (02) 9565 6185 or speak to your regular cardiologist or doctor.
Genetic testing can affect applications for life insurance. If you would more information visit the Centre for Genetics education website www.genetics.edu.au and click on fact sheet 23A: Life Insurance and Genetic Testing in Australia.
Will a diagnosis of Brugada syndrome change my lifestyle?
There are key recommendations that we advise people about when they are diagnosed with this condition. These guidelines help to reduce the risk of the most devastating outcome – sudden cardiac death.
- Avoid drugs that might aggravate Brugada syndrome and therefore worsen the condition. This list of drugs to avoid can be found at www.brugadadrugs.org You should check this list and consult your pharmacist prior to taking any medication including over-the-counter cough/cold/flu medicine.
- Fever (38°C and above) should be treated quickly with paracetamol as it can also aggravate Brugada syndrome.
- Avoid excessive alcohol intake as it can trigger events in people with Brugada syndrome.
- Regular check-ups with your cardiologist: It is important to monitor the progression of your condition and you should also report any new symptoms. This is because your cardiologist uses many different factors to determine whether you are at an increased risk of sudden death. Your risk of sudden death determines what mode of treatment will most benefit you. A defibrillator may be recommended if you are considered to be at high risk of sudden death.
- Surgical procedures: You should inform the attending doctor of your condition before any surgical or dental procedures.
- Consult with your GP or cardiologist before taking any new medications or supplements. It is important to talk to your doctor before taking any new medications, including alternative or natural medications e.g. herbal remedies. Some medications (even non-prescription medications) can aggravate Brugada syndrome and these should be avoided. A list is available at www.brugadadrugs.org
- Encourage relatives to be screened. As mentioned, siblings and children of an affected person have a 1 in 2 (50%) chance of being affected. Screening of relatives involves them seeing a cardiologist where they will have a physical examination and an ECG. The relatives needs to inform the doctor that there is a family history of Brugada syndrome to ensure no signs are missed. The Genetic Heart Disease Clinic held at the Sydney Heart Centre at RPA Hospital can screen relatives (appointments phone 02 9517 2011). Or you can find a specialist centre near you on our Cardiac Genetic Services page, contacting the Registry Coordinator on registry@centenary.org.au or (02) 9565 6185 or by speaking to your regular cardiologist or doctor.
Contacts:
If you have any further questions, please contact:
- Your local GP or cardiologist
- Your local Genetic Cardiac Service (see our Information Sheet on Genetic Cardiac Services)
- Australian Genetic Heart Disease Registry www.heartregistry.org.au , Tel: 02 9565 6185 or registry@centenary.org.au