For all women, there are a number of issues to consider when deciding whether to have a baby. However, for a woman with a genetic heart disease there are some important additional factors that need to be addressed to ensure a safe pregnancy for both the mother and baby. This information sheet will highlight some issues to consider. PDF Version
Key points:
- Multi-disciplinary care is essential, including your cardiologist, obstetrician and general practitioner.
- See your cardiologist before becoming pregnant, (or as early as possible when pregnant) to discuss your obstetric management in relation to your cardiac disease.
- Discuss whether your current medication is safe to use during pregnancy and breastfeeding.
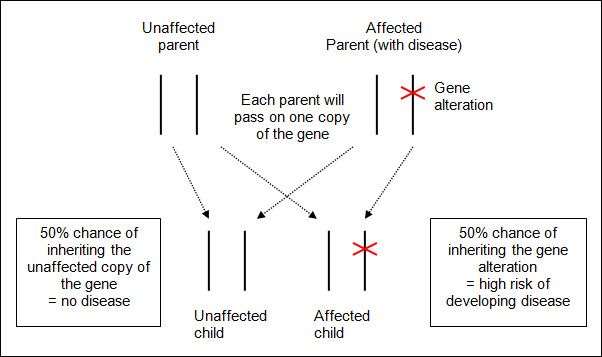
- Most genetic cardiomyopathies and arrhythmia diseases are inherited in an “autosomal dominant” manner. Each child will have a 1 in 2 (or 50%) chance of inheriting the genetic alteration (mutation), with both males and females equally affected.
- Most women with a genetic heart disease will have a successful and uneventful pregnancy.
See your cardiologist
Ideally, see your cardiologist prior to becoming pregnant, or as early as possible when you find out you are pregnant. Your cardiologist will want to check your heart function. This may involve some investigations such as an echocardiogram and electrocardiogram (ECG). These will give your cardiologist an opportunity to assess your clinical status and fitness for pregnancy, as well as give a baseline assessment for them to compare to in the future. Your cardiologist may refer you to a specialist centre for your follow-up during the pregnancy.
Medication
Some medications are not safe to take during pregnancy as the medication can cross the placenta and expose the baby to risks. Therefore you may need to change your medication. You should discuss your plans to conceive with your cardiologist so different medications can be prescribed (if necessary), that are safe to use during pregnancy. If you experience severe morning sickness, it may affect the absorption and effectiveness of your medications. It is also important to discuss the safety of medications in breastfeeding (if you intend to do so).
General Health
Before conception it is recommended that all women take 0.4-0.5 milligrams of folic acid daily. Folic acid (also called folate) reduces the chance of your baby being affected by spina bifida and other neural tube defects. This can be in the form of a pregnancy multivitamin but check the label to ensure you are receiving a sufficient dose. Ideally you should begin taking the folic acid 3 months prior to becoming pregnant.
As always, maintain a healthy and balanced diet. It is important to maintain regular exercise, such as 30 minutes of walking each day. While pregnant, listen to your body; you may require additional rest and if you have any concerns see your cardiologist, obstetrician or general practitioner.
Inheritance
Genetic heart disease can be inherited from a parent. Genetic heart diseases, such as cardiomyopathies and arrhythmia diseases, are inherited in an “autosomal dominant” manner. For specific information on your condition, see the relevant information sheet at www.heartregistry.org.au/patients-families/genetic-heart-diseases/.
Autosomal dominant means that you only need an alternation in one cardiac-related gene to be at-risk of developing the familial disease. It also means that both males and females are equally affected. If your genetic heart disease is inherited in an autosomal dominant manner, then each of your children has a 1 in 2 (or 50%) chance of inheriting the familial alteration and being at-risk of developing the disease in their lifetime. Below is a diagram depicting the process of autosomal dominant inheritance. If you would like to discuss the inheritance or testing options available in pregnancy, please speak to a genetic counsellor, at your local genetics service. www.genetics.edu.au/Genetics-Services/genetic-counselling-services
Pre-implantation Genetic Diagnosis and Genetic Testing in Pregnancy
Pre-implantation genetic diagnosis (PGD) is a scientific technique used in conjunction with in vitro fertilisation (IVF). PGD tests embryos to identify which embryos carry the familial mutation and which ones do not. Genetic testing during pregnancy is possible using chorionic villus sampling (CVS) or amniocentesis. If you would like more information regarding these options, we recommend contacting a genetic counsellor. www.genetics.edu.au/Genetics-Services/genetic-counselling-services
Symptoms during pregnancy
The heart is a muscle that is responsible for transporting blood, full of oxygen and nutrients, around the body. During pregnancy the volume of blood increases which causes the heart muscle to work harder. As a result some women may experience some dizziness, palpitations, shortness of breath and lethargy during pregnancy. Even women without a genetic heart disease can experience these symptoms during pregnancy, so monitor your symptoms and tell your doctor, especially if symptoms increase.
Delivery
In consultation with your cardiologist and obstetrician, a birth plan will be made regarding the type of delivery and optimum pain relief for labour. A vaginal delivery is the safest way to deliver the baby, even for women with a genetic heart disease. Epidural anaesthesia can also be used for pain control. Given the monitoring and possible complications that can be associated with childbirth, it is recommended that you deliver in a specialist obstetric and cardiac hospital.
After delivery
All women will recover from childbirth at slightly different rates. Some women with genetic heart disease may need to stay in hospital a little longer for monitoring. Some symptoms that may be experienced post childbirth include tiredness, breathlessness and swelling due to excess fluid. There is also a chance of arrhythmias, bleeding (haemorrhage) and clots (thrombosis) that your doctor will monitor and treat as needed.
Breastfeeding
As during pregnancy, some medications are not safe to consume while breastfeeding. Advise your cardiologist that you would like to breastfeed and alternative medications may be prescribed. In some cases women are advised not to breastfeed so that they receive their required and potentially life-saving medication. Always check with your cardiologist before making any changes to your medication, to ensure you are taking medication that is adequate for your treatment and safe for your baby.
Genetic Testing for Children
As your child will be at 1 in 2 (or 50%) chance of also developing a familial cardiomyopathy or arrhythmia disease it is natural to be concerned about them. However given you are aware of their risk, you will be able to ensure they are having the appropriate check-ups. Different conditions have different guidelines around when is the best time to perform clinical screening and genetic testing on children. For specific screening guidelines regarding your genetic heart disease talk to your cardiologist. Generally, genetic testing is not offered until a child is a teenager, so they can understand the implications of the test. However every family is different, so you can discuss this further with you cardiologist or genetic counsellor.